ADHD Is A Significant Risk Factor For PTSD
And not surprisingly, ADHD + PTSD can lead to addiction
PTSD and c-PTSD
Post Traumatic Stress Disorder (PTSD) is a mental health condition that’s triggered by a terrifying event. Symptoms may include flashbacks, nightmares and severe anxiety, as well as uncontrollable thoughts about the event.
Complex PTSD (c-PTSD) is caused by ongoing trauma, or trauma that was previously ongoing for months or years, often in childhood.
trauma with a lowercase ‘t’
Those are the definitions of PTSD and c-PTSD according to the DSM-V and the American Psychiatric Association (APA). There is also what many of us in the neurodivergent community call trauma with a lowercase ‘t’.
Dr. Sharon Saline describes this as “death by a thousand paper cuts”, the constant criticism and correction neurodivergent people experience daily throughout their entire lives. This can cause a type of complex trauma that can lead to hypersensitivity, perfectionism, and anxiety.

Trigger Warning
I will not directly discuss any traumatic events, but reading about PTSD or c-PTSD can be triggering in itself. It is difficult just writing about the topic, even from an over-intellectualizing distance without getting into specifics.
Please practice good self-care and do not read if you feel the content may do you more harm than good.
As always, my articles are intended to be informative and supportive, but are not intended as individual mental health advice, and cannot replace the advice of a medical professional.
The connection between ADHD and PTSD
ADHD is a significant risk factor for PTSD. In the general population, the rate of PTSD is estimated to be about 1.6%, whereas it’s estimated that around 10% of people with ADHD also have PTSD.
This is largely because people with ADHD also have a higher number of Adverse Childhood Experiences (ACEs). The American Academy of Pediatrics estimates that 17% of children with ADHD have experienced four or more ACEs compared to 6% of children without ADHD.
Recent research has indicated that delayed identification, diagnosis, and provision of supports may further increase the risk of trauma and childhood adversity.
The Adverse Childhood Experiences questionnaire includes questions on the following 10 traumatic experiences.
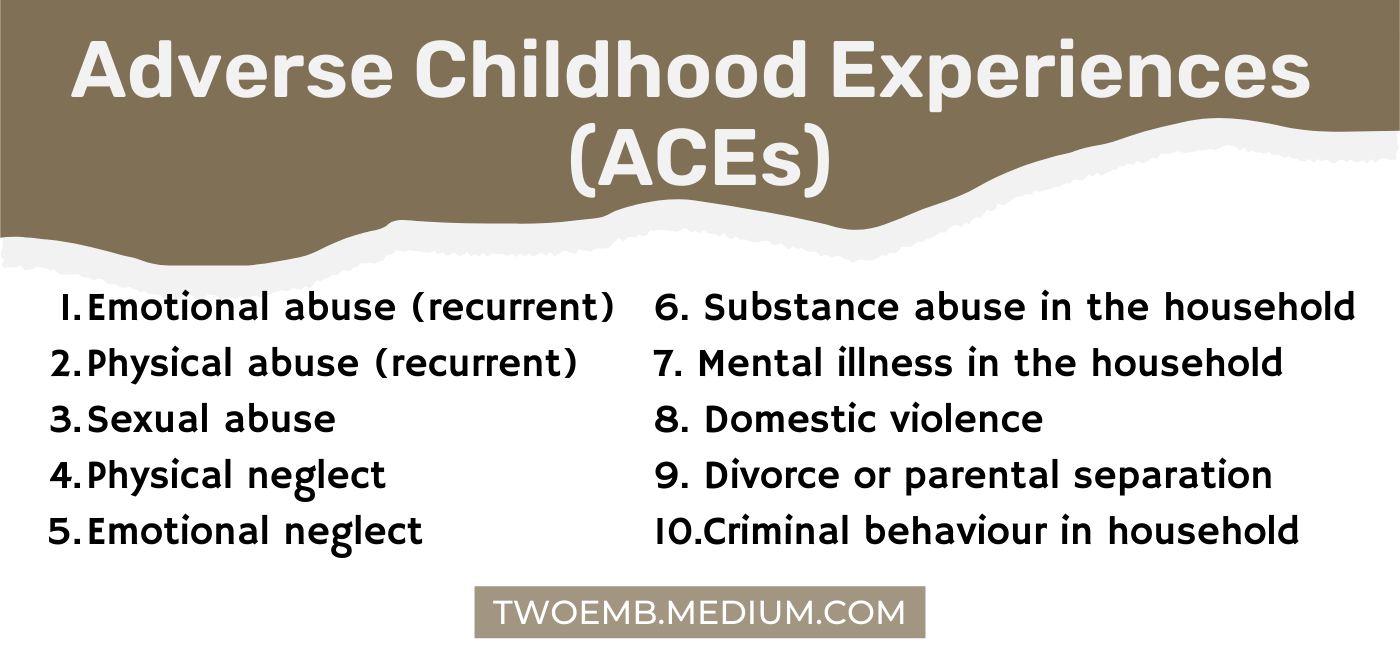 Image created by author — (list from Harris, 2018)
Image created by author — (list from Harris, 2018)
As you might guess, the higher the number of ACEs, the higher the negative health and psychological outcomes.
Frustratingly, the research tells us that having ADHD increases our risk of experiencing trauma, but doesn’t really explain why.
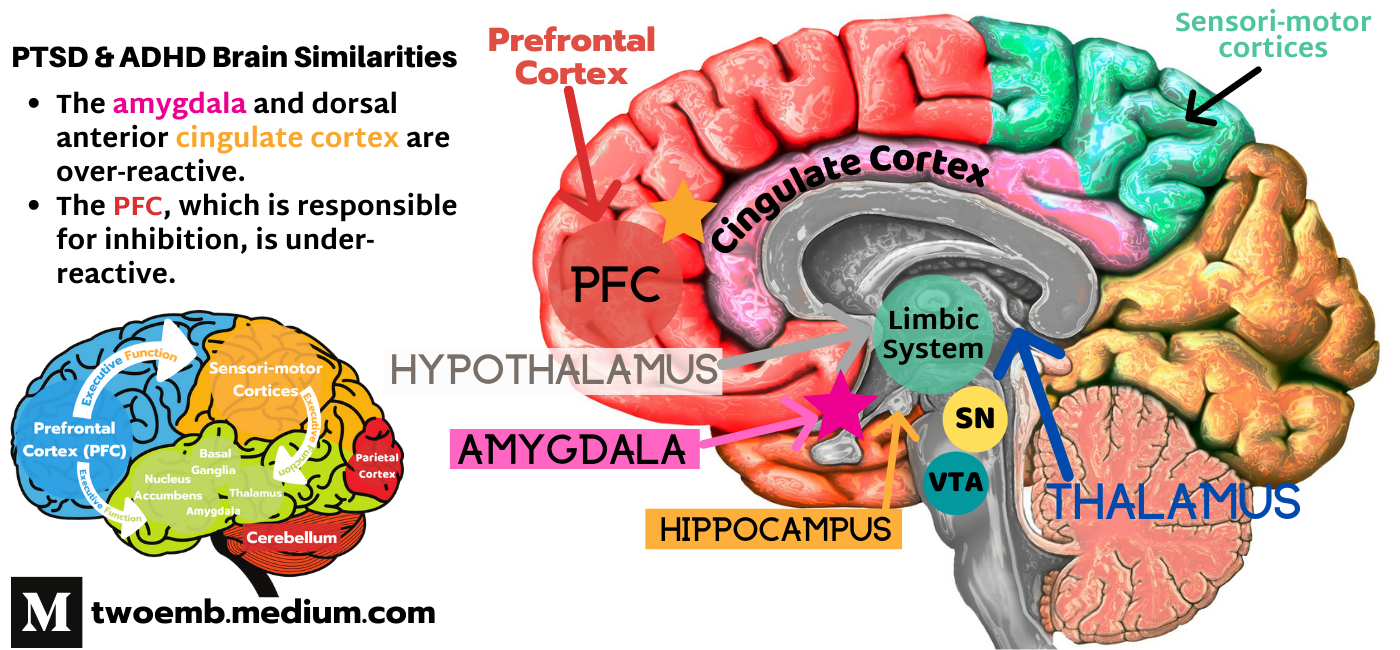
One theory posits that because some of the brain changes that occur in PTSD are similar to those found in ADHD, people with ADHD are not only more vulnerable to experiencing trauma, they are also more susceptible to developing PTSD as a result.
There is preliminary research shown irregularities in dopaminergic neurotransmission and prefrontal cortex dysfunction in both ADHD brains and the brains of people with PTSD.
The amygdala and dorsal anterior cingulate cortex are hyper-reactive in both PTSD and ADHD, leading to increased emotional intensity and exaggerated fear response. These abnormalities are also likely to underlie the attentional bias towards threat, impaired emotion regulation and persistence of fear memories in this disorder.
The prefrontal cortex (PFC) is the command centre for the brain. Its job is to evaluate and delegate. When the PFC is not functioning properly, we can be over- or under-reactive in many different ways.
With both ADHD and PTSD, the PFC is under-reactive, so it doesn’t inhibit or prevent other areas of the brain from over-reacting. The amygdala, which is a primary part of the limbic system, is largely responsible for our emotions.
When the PFC is under-active and the amygdala is over-reactive, this makes it much more difficult to regulate our emotional responses. This includes our overt behaviours, but also our thoughts and memories. These processes are thought to contribute to difficulties suppressing intrusive thoughts and distressing memories.
Being impulsive and having a less mature prefrontal cortex may also make us more vulnerable to being victimized. Challenging and externalizing childhood behaviours, such as irritability, antisocial behaviour, and hyperactivity have also been found to increase a child’s risk of trauma.
One more thing…
Another not-so-shocking connection I found while doing this research was that a significant proportion of patients with PTSD and AUD (alcohol use disorder) have a high level of ADHD symptoms.
The inverse has also been demonstrated. A much greater percentage of patients with both ADHD and SUD had PTSD, and a greater percentage of patients with SUD have ADHD.
A 2020 study of over 500 people receiving inpatient treatment for alcohol abuse found that 20% of their patients met the criteria for ADHD (compared to an estimated 4% of adults in the general population), and of those patients, 84% also met the criteria for PTSD.
It’s not surprising when you know people with ADHD already have a higher risk of developing addictions, add to that the fact that we have an increased risk of being victims of trauma, and subsequently experiencing symptoms of PTSD.
What can we do with this information?
First and foremost, if you have ever experienced trauma: It is not your fault.
Abusers and perpetrators look for certain vulnerabilities in people so they can take advantage of them. It is not our fault that we were born with brains that make us more vulnerable.
Secondly, knowledge can help prevent further trauma and protect others moving forward. If you work with children, have children, or have vulnerable people in your life, it helps to know how and why, so that you can help them develop tools and skills to keep themselves safe.
More importantly, you can be better prepared to spot people who might put others at risk, or take advantage of those vulnerabilities.
The onus is always on the adults, and the responsibility is always on the perpetrator, never the victim. (And yes, I can say and type that with a straight face, or tell that to anyone other than myself, while also convincing myself that it is still my fault, those rules don’t apply to me).
There are a lot of good resources out there, both for working to prevent trauma and protect children, but also help for those healing from trauma. I am not there yet, so I can’t offer you many words of encouragement (sorry), I am only beginning my journey.
What I can offer is the message that you’re not alone. That’s the best I can do for now.
© Jillian Enright
Related Stories
How Executive Dysfunction Impacts Daily Life
ADHD Increases Our Risk for Addictions
Impulsivity: It’s A Neurodivergent Thing.

References
American Academy of Pediatrics. (2014, May 6). Study finds ADHD and trauma often go hand in hand. ScienceDaily. Retrieved October 21, 2021 from www.sciencedaily.com/releases/2014/05/140506074719.htm
Antshel, K. M., Kaul, P., Biederman, J., Spencer, T. J., Hier, B. O., Hendricks, K., & Faraone, S. V. (2013). Posttraumatic stress disorder in adult attention-deficit/hyperactivity disorder: clinical features and familial transmission. The Journal of clinical psychiatry, 74(3), e197–e204. https://doi.org/10.4088/JCP.12m07698
Biederman, J., Petty, C., Spencer, T. J., Woodworth, K. Y., Bhide, P., Zhu, J., & Faraone, S. V. (2014). Is ADHD a risk for posttraumatic stress disorder (PTSD)? Results from a large longitudinal study of referred children with and without ADHD, The World Journal of Biological Psychiatry, 15(1), 49–55. https://doi.org/10.3109/15622975.2012.756585
Bolstad, I., Lien, L., & Bramness, J. G. (2021). ADHD symptoms as risk factor for PTSD in inpatients treated for alcohol use disorder. Psychiatry Research, 300, 113904. https://doi.org/10.1016/j.psychres.2021.113904
Brown, N. M., Brown, S. N., Briggs, R. D., Germán, M., Belamarich, P. F., Oyeku, S. O. (2017). Associations Between Adverse Childhood Experiences and ADHD Diagnosis and Severity. Academic Pediatrics, 17(4), 349–355. https://doi.org/10.1016/j.acap.2016.08.013
Burke, H. N. (2018). The deepest well: Healing the long-term effects of childhood adversity. Houghton Mifflin Harcourt.
Center for Substance Abuse Treatment (2014). Trauma-Informed Care in Behavioral Health Services. Substance Abuse and Mental Health Services Administration (US). (Treatment Improvement Protocol (TIP) Series, №57.) Exhibit 1.3–4, DSM-5 Diagnostic Criteria for PTSD. [Online]. https://www.ncbi.nlm.nih.gov/books/NBK207191/box/part1_ch3.box16
Cloitre, M. (2020). ICD-11 complex post-traumatic stress disorder: Simplifying diagnosis in trauma populations. The British Journal of Psychiatry, 216(3), 129–131. https://doi.org/10.1192/bjp.2020.43
El Ayoubi, H., Brunault, P., Barrault, S., Maugé, D., Baudin, G., Ballon, N., & El-Hage, W. (2021). Posttraumatic Stress Disorder Is Highly Comorbid With Adult ADHD in Alcohol Use Disorder Inpatients. Journal of Attention Disorders, 25(11), 1594–1602. https://doi.org/10.1177/1087054720903363
Koenen, K., Moffitt, T., Poulton, R., Martin, J., & Caspi, A. (2007). Early childhood factors associated with the development of post-traumatic stress disorder: Results from a longitudinal birth cohort. Psychological Medicine, 37(2), 181–192. https://doi.org/10.1017/S0033291706009019
Luderer, M., Reinhard, I., Richter, A., Kiefer, F., Weber T. (2020). ADHD Is Associated with a Higher Risk for Traumatic Events, Self-Reported PTSD, and a Higher Severity of PTSD Symptoms in Alcohol-Dependent Patients. European Addiction Research, 26, 245–253. https://doi.org/10.1159/000508918
Lugo-Candelas, C., Corbeil, T., Wall, M., Posner, J., Bird, H., Canino, G., Fisher, P. W., Suglia, S. F., & Duarte, C. S. (2021). ADHD and risk for subsequent adverse childhood experiences: understanding the cycle of adversity. Journal of child psychology and psychiatry, and allied disciplines, 62(8), 971–978. https://doi.org/10.1111/jcpp.13352
Mahan, A. L., & Ressler, K. J. (2012). Fear conditioning, synaptic plasticity and the amygdala: implications for posttraumatic stress disorder. Review Special Issue: Neuropsychiatric Disorders, 35(1), 24–35. https://doi.org/10.1016/j.tins.2011.06.007
Martínez, L., Prada, E., Satler, C., Tavares, M. C., & Tomaz, C. (2016). Executive Dysfunctions: The Role in Attention Deficit Hyperactivity and Post-traumatic Stress Neuropsychiatric Disorders. Frontiers in psychology, 7, 1230. https://doi.org/10.3389/fpsyg.2016.01230
Pitman, R., Rasmusson, A., Koenen, K. et al. (2012). Biological studies of post-traumatic stress disorder. Nature Reviews Neuroscience 13, 769–787. https://doi.org/10.1038/nrn3339
Saline, S. (2018). What Your ADHD Child Wishes You Knew: Working together to empower kids for success in school and life. TarcherPerigee.
Spencer, A. E., Faraone, S. V., Bogucki, O. E., Pope, A. L., Uchida, M., Milad, M. R., Spencer, T. J., Woodworth, K. Y., & Biederman, J. (2016). Examining the association between posttraumatic stress disorder and attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. The Journal of clinical psychiatry, 77(1), 72–83. https://doi.org/10.4088/JCP.14r09479